Sputum cultures detect the presence of bacteria which have the potential to cause infection. These bacteria in the sample are identified and their susceptibility to various antibiotics is assessed to help choose the most appropriate antibiotic (antimicrobial) treatment.
Sputum is the thick mucus or phlegm that is coughed up from the lower respiratory tract; it is not saliva or spit. If a sample is mostly saliva, the microorganisms grown in culture will not necessarily be those causing the infection. Furthermore, the presence of saliva and bacteria from the mouth in a sputum sample make it more difficult to identify disease-causing bacteria in the lungs.
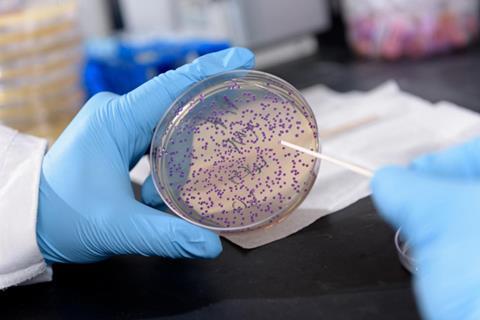
Sputum is broken up with a substance called mucolyse. This ensures that the bacteria present in the sample is evenly distributed throughout the sample. Once a sputum sample is fully homogenised it is placed on appropriate nutrient media and incubated under conditions which simulate body temperature. The media encourages bacteria to grow which allows further testing and identification. Sputum is not normally free of bacteria, so when a person has a bacterial respiratory infection, there will typically be both normal and infection-causing bacteria present.
The next step is to identify the different types of bacteria present and categorise them as normal or potential infection-causing bacteria. Differentiation is performed by a trained scientist and suspected infection causing bacteria are followed up with confirmatory tests.
'Antimicrobial susceptibility testing’ is frequently used to find out whether they are likely to respond to particular antibiotics and determine the best treatment option.
The sputum culture and susceptibility testing all contribute to helping the doctor find out what has caused the infection and what antibiotic might be used to treat it.
Some infectious agents cannot be grown and identified with a routine bacterial sputum culture, so that other tests, such as an AFB smear and culture, fungal culture, or viral PCR testing, may be requested in addition to or instead of a routine culture.
Acid-Fast Bacillus (AFB) Testing
The test looks for the presence of bacteria called acid-fast bacilli (AFB) which are rod shaped bacteria that can be seen and counted under the microscope in a specially stained sample on a glass slide, called an AFB smear. The most common AFB are of a type called mycobacteria.
Mycobacterium tuberculosis complex is the most common species of mycobacteria, and is the most infectious. Most AFB smears and cultures are collected because the doctor suspects that the patient has TB. Other few mycobacteria that have been identified cause infections in humans. They include:
Several smears from different samples should be checked for AFB since the number of bacilli may vary day to day. If acid-fast bacilli are present on any of the smears, a mycobacterial infection is likely. Since M. tuberculosis is the most common cause of respiratory infections with mycobacteria, a provisional diagnosis of TB can be made but other follow-up testing must be done to positively identify the acid-fast bacilli as either M. tuberculosis, or another mycobacteria species.
Body fluids such as urine or CSF are used for AFB cultures at the same time as the smears. The cultures are used to grow AFB in the laboratory. Since mycobacteria grow slowly, positive identification of the species that is/are present may take days to several weeks, while negative results (no mycobacterial growth) can take up to 6 to 8 weeks to confirm.
Rapid testing
Several other testing methods, based on genetic components of mycobacteria, have been developed to help decrease the amount of time necessary to diagnose tuberculosis. These include genetic probes and molecular TB testing. In less than 24 hours these tests can amplify/replicate pieces of the bacterial genetic code. These methods are suitable for respiratory samples and must be confirmed with an AFB culture, but they do provide the doctor with a quick answer, allowing him to isolate potentially infectious patients and reduce the spread of the disease.
Rapid testing using molecular amplification of bacterial DNA is becoming more common and some laboratories may offer a rapid PCR (polymerase chain reaction) test. Some of these tests can also provide information on the susceptibility of the bacteria if present (generally only one or two antibiotics, not the full panel) and only if the test is positive. Please note that a negative rapid test does not rule out a diagnosis and it does not replace the need to culture the sample. Multiple samples for monitoring treatment may be still required.

Blood cultures are performed to detect and identify bacteria and yeasts (a type of fungus) in the blood. Infections of the bloodstream are caused most commonly by bacteria (bacteraemia), but can also be caused by a fungus (fungaemia) or a virus (viraemia). The source of the infection is typically a specific site within the body. If the immune defences and white blood cells cannot keep the infection localised at its source it may spread to the bloodstream. When the body has an excessive response to this, causing damage to the organs of the body and stopping them functioning properly, this is known as sepsis. If the sepsis also causes reduced blood flow through the organs of the body, this is referred to as septic shock, which is a serious, overwhelming and often fatal illness.
Blood cultures are also important in the diagnosis of several other conditions. Endocarditis, an inflammation and infection of the lining of the heart and/or the heart valves, can result from a bloodstream infection. People who have artificial heart valves or artificial joints have a higher risk of infection following surgery, although these infections are not common. The direct contamination of the blood from “dirty needles” with intravenous drug use, or potentially from intravenous catheters or surgical drains can lead to bloodstream infections. Similarly, anyone with an immune system which is not working properly due to underlying disease (for example, leukaemia or HIV/AIDS) or drug therapy (for example, immunosuppressive agents) has a higher chance of bloodstream infections.
If your blood culture is positive, the specific bacteria causing the infection will be identified and antibiotic susceptibility testing will be done to tell your doctor which antibiotics will be effective for treatment. If yeasts are causing the infection, treatment will be given that is appropriate for fungal infections.
Urine Culture

Urine is one of the body’s waste products. It is produced in the kidneys and collected in the bladder until a person urinates. Normally, the urine does not contain significant numbers of any microorganism. However, if bacteria or yeast are introduced into the urinary tract, they can multiply and cause a urinary tract infection, called a UTI.
Most UTIs are caused by Escherichia coli (E. coli), one of the most common bacteria found in the human bowel. Other frequently identified bacteria are Proteus, Klebsiella, and Staphylococcus saprophyticus.
If bacteria are detected in the urine, they will then be tested for their antibiotic susceptibility so that an effective treatment can be administered.
A “mid-stream” urine sample is necessary for a culture so bacteria present around the urethra and on the hands are not introduced. The procedure for collecting a clean “mid-stream” includes the following steps:
Uncontaminated specimens can also be obtained from catheterised patients following the same hygienic procedures for the end of the catheter. Urine can also be collected directly from the bladder using a needle and syringe in a process known as a suprapubic aspiration, but this is usually reserved for infants and young children where it has been difficult to obtain a reliable mid-stream urine sample.
A sample of the urine is then spread across the surface of one or more agar plates and placed in an incubator at body temperature overnight. If there is no growth on the agar plates at the end of that time, the culture is considered negative for significant number of microorganisms that could cause an infection. If bacteria or yeast are present, the total number of organisms is counted (colony count), and they are identified by additional biochemical or molecular testing. Further tests will determine which antibiotics are likely to be effective in treating the infection.
Generally none; however, you may be instructed not to urinate for at least an hour before the test and/or to drink a glass of water 15-20 minutes before sample collection. This will help to ensure that you can produce enough urine for the sample. Follow the instructions provided for collecting a clean catch urine sample.
Stool Culture

The stool culture is a test that allows the detection and identification of pathogenic (harmful) bacteria in the stool. In the laboratory, a small amount of a fresh faecal sample is applied to a variety of nutrient media (thin layers of gelatin like material in sterile covered plastic dishes). These media are selective, each encourages the growth of some bacteria and discourages the growth of others. Once inoculated, the media are incubated and checked daily for bacterial growth. Bacteria that are present in the stool grow as colonies that look like dots on the surface of the gel. The physical characteristics of the colonies - their shape, colour, and some of their chemical properties are unique to each type of bacteria and allow them to be differentiated.
The bacteria in the stool are representative of the bacteria that are present in the gastrointestinal tract and it is a far from sterile environment. Bacteria and fungi called “normal flora” inhabit the gastrointestinal tract. They play an important role in the digestion of food and they form a protective barrier against the growth of other pathogenic bacteria. Normal flora are usually in balance but sometimes one, such as Clostridium difficile, will become pathogenic by overgrowing. This upsets the balance of the normal flora and may lead to the production of toxins that can irritate and damage the intestinal tract. Bacterial overgrowth is usually a side effect of the administration of broad-spectrum antibiotics (which depresses the growth of the other normal flora) but it may also be seen in patients who are immunocompromised.
Other pathogenic bacteria are usually brought into the body when someone eats food or drinks water that has been contaminated. This may include raw or undercooked eggs, poultry or beef, unpasteurised milk, and contaminated water from lakes, streams, and (occasionally) from community water supplies. Those that travel outside the U.K., especially to developing nations, may face a greater risk of being exposed to pathogenic bacteria. Some of these bacteria may be “true pathogens” while others are strains of gastrointestinal bacteria that are normal flora for the locals, but cause gastrointestinal distress to the tourist. Visitors may become infected by eating or drinking anything that has been contaminated with the bacteria (things as simple as tap water, ice cubes in a drink, a fresh salad etc).
The most common symptoms of a pathogenic bacterial infection are prolonged, bloody diarrhoea, mucous in stool, abdominal pain, and nausea. This is usually a self-limiting illness and doesn’t require antibiotics. If diarrhoea lasts more than a few days, it may lead to dehydration and electrolyte imbalance - dangerous conditions in children and the elderly. Dehydration can cause symptoms such as: thirst, dry skin, fatigue, light-headedness, and fever. Severely affected patients may require hospitalization to replace lost fluids and replace lost electrolytes. A serious complication that may occasionally arise is haemolytic uraemic syndrome. It is most frequently seen in children infected with Eschericia coli 0157:H7 and may lead to the destruction of red blood cells and to kidney failure.
The most common pathogenic bacteria and their most frequently encountered sources include:
Others include: Staphylococcus aureus, Clostridium difficile and strains of Yersinia and Vibrio.
Bacterial Wound Culture
A bacterial wound culture is a test that is used to detect and identify pathogenic bacteria in a potentially infected wound. Wounds may be superficial breaks in the skin such as scrapes, cuts and scratches or may involve deeper tissues such as incisions, bites, punctures or burns. Any wound may become infected with a variety of bacteria. A culture helps to determine which type or types of bacteria are causing an infection, and which antibiotic would best treat the infection and help heal the wound.
A culture is performed by collecting a sample of fluid, cells or tissue from the wound and placing it on or in appropriate nutrient media. The media encourages the growth of bacteria that may be present, allowing for further testing and identification. Typically if a person has a wound infection, there will either be a pure culture of the microorganism - only one kind will be found, or one type will predominate. In some cases, for instance with a human or animal bite, there may be several pathogens present. Since wounds may be superficial or involve deep tissue, they may harbour different types of bacteria that have different requirements for growth. Some bacteria infecting a wound may require air for growth (aerobic) while some require a no-oxygen or reduced-oxygen environment (anaerobic or microaerophilic). Care must be taken when handling the samples so that their growth is encouraged and the probability of their detection and identification are optimized.
The next step in the process is to identify the different types of microorganisms present. Identification is a step-by-step process that may involve many tests and evaluations performed on the bacteria found growing in the culture. One such test, the Gram stain, involves smearing individual colony types onto glass slides and treating them with a special stain. Under the microscope, the bacteria can be classified into Gram-positive and Gram-negative organisms and by shape into cocci (spheres) or rods. With this information and additional biochemical tests, the types of bacteria present can be identified.
For many of the pathogens identified in the wound culture, antimicrobial susceptibility testing is required to guide treatment and to determine whether the strain of bacteria present is likely to respond to specific antibiotics. In order to do this, a pure culture (isolate) of the identified bacteria must be available, which may require additional time in the laboratory to separate and identify each bacterial species.
The wound culture, Gram stain test, and susceptibility testing all contribute to inform the doctor which pathogen(s) are present and what antibiotic therapy is likely to inhibit their growth.
These tests are used to help diagnose, evaluate, and monitor people suspected of having Acute Coronary Syndrome (ACS). |
||||||
| MARKER | WHAT IT IS | TISSUE SOURCE | REASON FOR INCREASE | TIME TO INCREASE | TIME BACK TO NORMAL | WHEN/HOW USED |
Cardiac Troponin |
Regulatory protein complex; two cardiac-specific isoforms: T and I | Heart | Injury to heart | 3 to 4 hours | Remains elevated for 10 to 14 days | Diagnose heart attack, risk stratification, assist in deciding management, assess degree of damage |
High-sensitivity cardiac troponin |
Same as above, just measures the same protein at a much lower level | Heart | Injury to heart | Within 3 hours of onset of symptoms | Same as above | Same as above; may also be elevated in stable angina and people without symptoms and indicates risk of future cardiac events (e.g., heart attacks) |
CK |
Enzyme; total of three different isoenzymes | Heart, brain, and skeletal muscle | Injury to skeletal muscle and/or heart cells | 3 to 6 hours after injury, peaks in 18 to 24 hours | 48 to 72 hours, unless due to continuing injury | Frequently performed in combination with CK-MB; sometimes to detect second heart attack occurring shortly after the first |
CK-MB |
Heart-related isoenzymes of CK | Heart primarily, but also in skeletal muscle | Injury to heart and/or muscle cells | 3 to 6 hours after heart attack, peaks in 12 to 14 hours | 48 to 72 hours, unless new or continuing damage | Less specific than troponin, may be ordered when troponin is not available |
Myoglobin |
Oxygen-storing protein | Heart and other muscle cells | Injury to muscle and/or heart cells | 2 to 3 hours after injury, peaks in 8 to 12 hours | Within one day after injury | Used less frequently; sometimes performed with troponin to provide early diagnosis |