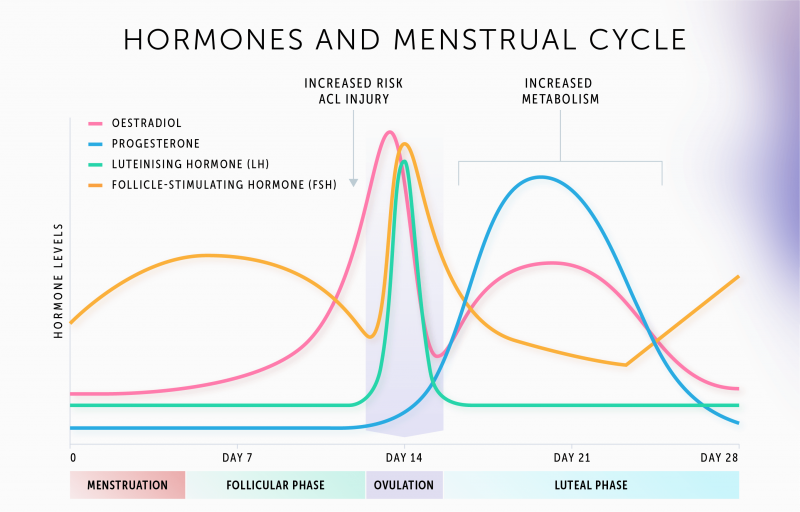

Follicle-stimulating hormone (FSH) helps control a woman’s menstrual cycle and the production of eggs. In men, it regulates the production and transportation of sperm.
For women, an FSH test is done on the third day of the menstrual cycle and is used to evaluate egg supply. For men, the test is used to determine sperm count.
Estradiol is an important form of estrogen. An estradiol test is used to measure a woman’s ovarian function and to evaluate the quality of the eggs. Like FSH, it is done on the third day of a woman’s menstrual cycle.
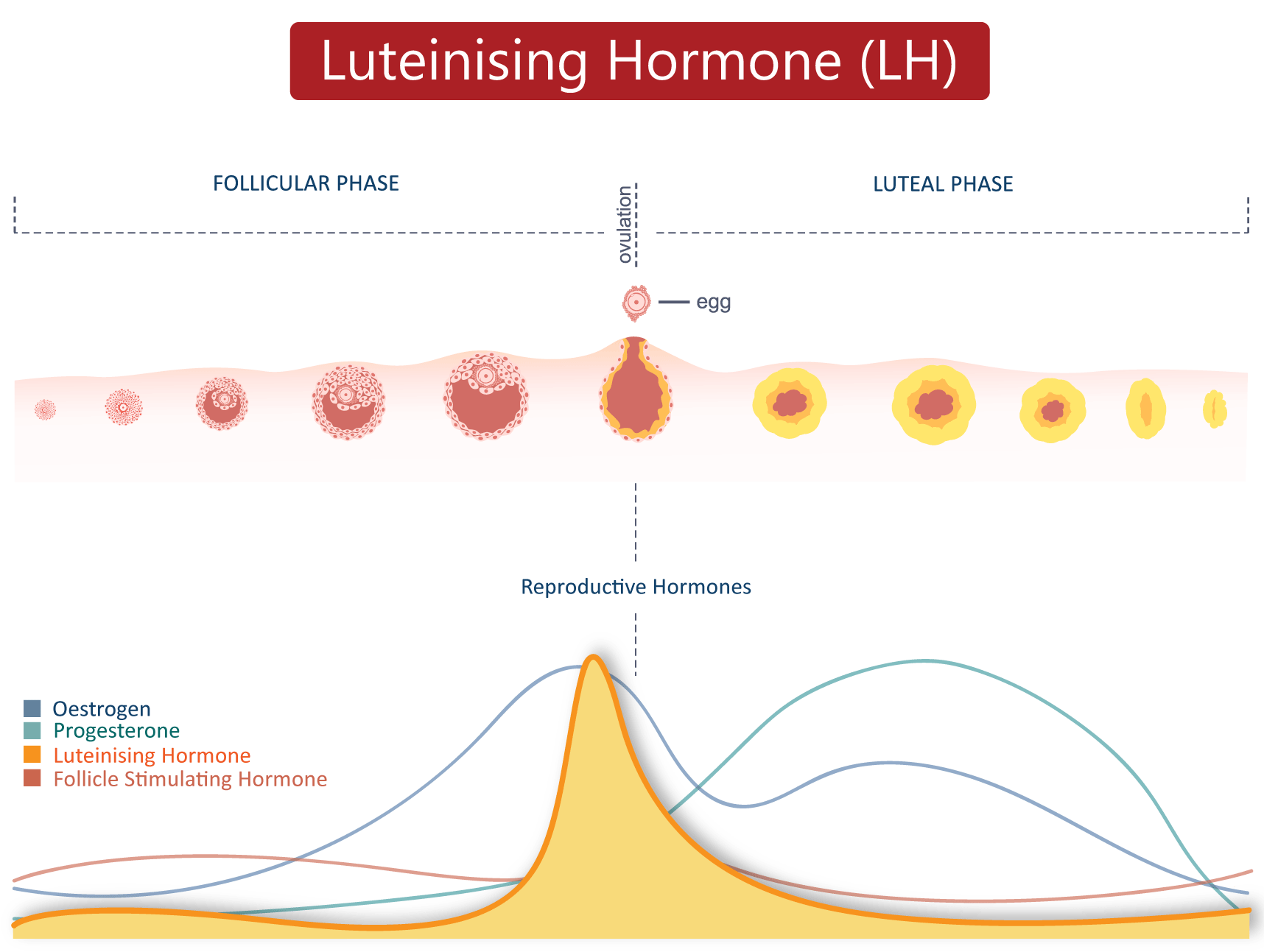
In women, luteinizing hormone (LH) is linked to ovarian hormone production and egg maturation. In men, it stimulates the hormone testosterone which affects sperm production.
An LH test is used to measure a woman’s ovarian reserve (egg supply) and a man’s sperm count. It is done during a woman's menstrual cycle to see if she is ovulating
Progesterone is a female hormone produced by the ovaries during ovulation. It causes the endometrial lining of the uterus to get thicker, making it receptive for a fertilized egg.
A serum progesterone test is used to determine if ovulation is occurring. Since progesterone levels increase towards the end of a woman’s cycle, the test is done during the luteal phase of the menstrual cycle (just before her period starts).
The hormone prolactin is made by the pituitary gland and causes milk production.
In women, a prolactin test is done to find out why they are not menstruating, or why they are having infertility problems or abnormal nipple discharge. The test is done in men when there is a lack of sexual desire, difficulty getting an erection, or if there might be a problem with the pituitary gland.
Testosterone is probably the most well-known androgen and it affects the sexual functioning of both men and women.
In men, an androgen test is used to find the cause of a low sex drive, the inability to get an erection, or infertility. In women, it is used to determine the cause of irregular periods or a low sex drive.

The test measures a hormone called anti – Müllerian hormone (AMH). This hormone is very important during the development of the male foetus as it is essential for the formation of male reproductive organs.
In males, AMH is generated within cells in the testes. AMH is detectable at birth in males and levels rise rapidly in infancy. After puberty, the levels of AMH decline in men.
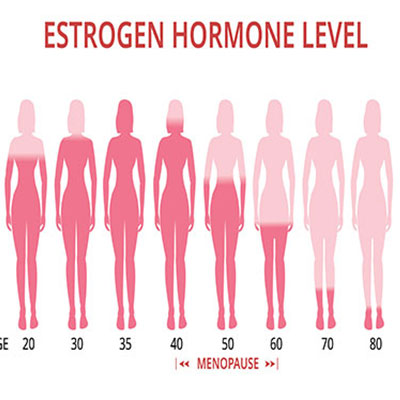
In females, small amounts of AMH are produced by developing follicles in the ovaries. At birth and in childhood the level of AMH in girls is very low but increases significantly at puberty reaching a peak in early adulthood. As women age, the number of follicles (which produce AMH) decreases and so the level of AMH declines and becomes undetectable after the menopause. AMH levels in women therefore reflect the declining ovarian function, and its measurement is said to indicate ovarian reserve.
Testosterone Test
Testosterone is a steroid hormone (androgen) made by the testes and adrenal glands in males, and by the peripheral tissues, adrenal glands and ovaries in females.
In males, testosterone has a role in reproductive health, facial and body hair, muscle mass and sex drive. In females, testosterone levels are about one tenth of those in males. In combination with oestrogen, testosterone in females has a role in bone health, sex drive and reproductive health.
Semen Analysis
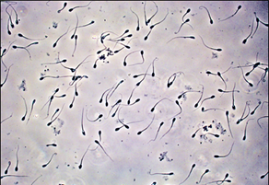
A semen analysis measures the quantity and quality of the fluid released from the penis during ejaculation. It evaluates both the liquid portion, called semen, and the microscopic moving cells, called spermatozoa (sperm).
Semen is the turbid, whitish liquid that contains sperm and the products from several glands. It is normally fairly thick after ejaculation and then becomes thinner within ten to thirty minutes. Sperm are the reproductive cells in semen that have a head and a tail. Each sperm contains one copy of each chromosome (all of the male’s genes). Sperm should be progressively motile (can move forward independently) and this allows them to travel to and fuse with the female’s egg, resulting in fertilisation. In each semen sample, there should be millions of sperm and varying amounts of other substances that support fertilisation.
A typical semen analysis could measures:
Additional tests may be performed if semen is abnormal, such as a test for antisperm antibodies. If assisted reproductive technology is contemplated, e.g. in vitro fertilisation (IVF), sperm function tests may also be performed.
Most laboratories require samples to be collected at the hospital as the semen needs to be examined within one hour after ejaculation for a fertility semen analysis. Semen is collected in a dedicated private area with a locked door. The man masturbates and collects the semen in a sterile specimen container.
Some men, for religious or other reasons, might want to collect semen during the act of intercourse, using a condom. If this is the case, the man should ask doctor to provide a silastic condom which is specifically made to be non-toxic to sperm. Do not use standard condoms as these are usually spermicidal.
Sperm are very temperature sensitive. If the sample is collected at home, the sample should be kept next to the body during transportation. It should not be left at room temperature and should not be refrigerated or heated. The sample must be delivered to the lab within one hour for analysis.
In order for the test to be reliable, you need to abstain from masturbation or sex for two to seven days before the sample is collected. You should follow the instructions given to you by the laboratory or your doctor. You should not collect the sample via intercourse or oral stimulation, as this can contaminate the sample. The penis and genitals should be thoroughly cleaned, rinsed and dried before sample production. No lubricants should be used, as these can be toxic to sperm.